
In a groundbreaking development in oncology imaging, researchers have unveiled the potential of a novel positron emission tomography/computed tomography (PET/CT) tracer, ^18F-FAPI-04, to sensitively detect radiation esophagitis (RE) in patients suffering from locally advanced esophageal squamous cell carcinoma (LA-ESCC). This investigation, recently published in BMC Cancer, represents a significant leap forward in non-invasive monitoring of treatment-induced esophageal inflammation during concurrent chemoradiotherapy (CCRT), a common therapeutic approach for LA-ESCC.
Radiation esophagitis is a frequently encountered complication that arises during radiotherapy of esophageal cancers. It involves inflammatory damage of the esophageal lining, often resulting in pain, swallowing difficulty, and potentially severe morbidity. Despite its clinical importance, early detection and accurate assessment of RE severity remain challenging. Conventional diagnostic methods primarily rely on symptomatic evaluation and endoscopy, which can be invasive and subjective. The advent of molecular imaging agents like ^18F-FAPI-04 PET/CT offers promise for objective, early visualization of radiation-induced tissue changes.
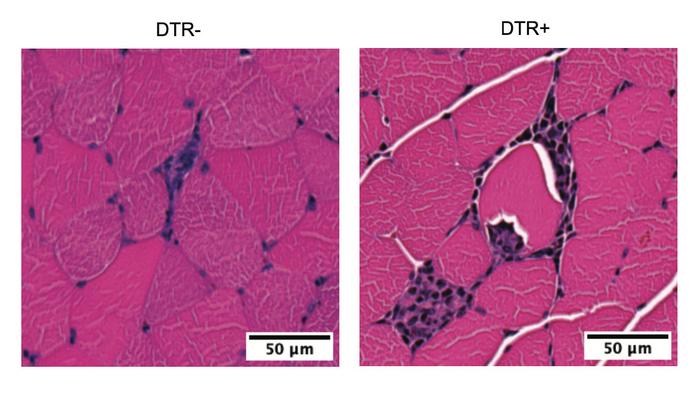
Fibroblast activation protein (FAP) is a cell surface serine protease selectively overexpressed in activated fibroblasts within the tumor microenvironment and sites of fibrosis or tissue injury. The tracer ^18F-FAPI-04 binds specifically to FAP, allowing PET/CT imaging to visualize fibroblast-driven processes. The researchers hypothesized that this tracer could identify fibroblast activation secondary to radiation-induced esophageal injury, thus providing an innovative biomarker for early RE detection.
This prospective study enrolled thirty patients diagnosed with locally advanced esophageal squamous cell carcinoma undergoing CCRT. The inclusion criteria ensured a homogenous patient cohort receiving similar radiation protocols. PET/CT imaging sessions using ^18F-FAPI-04 were conducted both before starting radiotherapy and at intervals during treatment. This longitudinal imaging approach allowed the investigators to monitor dynamic changes in tracer uptake correlating with radiation exposure.
Radiation Therapy Oncology Group (RTOG) criteria were used to clinically grade the severity of radiation esophagitis on a weekly basis. These assessments served as the clinical standard against which imaging findings were compared. The key imaging metric analyzed was the target-to-background ratio in blood (TBR_blood), representing the selective uptake of ^18F-FAPI-04 in esophageal tissue relative to background blood signal. The study further analyzed the change in this ratio (ΔTBR_blood) from baseline values to gauge treatment-induced alterations.
Findings revealed a statistically significant elevation in TBR_blood during radiotherapy in patients who developed RE compared to those who did not. More strikingly, the magnitude of ΔTBR_blood was strongly associated with the onset and severity of esophageal inflammation. Patients who progressed to grade 3 RE exhibited notably higher tracer uptake changes than those with lower grades of esophagitis. These correlations suggest that ^18F-FAPI-04 PET/CT imaging can serve as a sensitive biomarker reflecting the biological impact of radiation on esophageal tissues.
Multivariate logistic regression analyses were performed to account for potential confounders and identify independent predictors of RE. The ΔTBR_blood emerged as a significant and robust factor in detecting both any grade of RE and particularly severe (grade 3) esophagitis. This implies that alterations in fibroblast activation visualized by ^18F-FAPI-04 PET/CT could fundamentally inform risk stratification and clinical management.
The ability to visualize fibroblast activation in real time represents a paradigm shift from traditional imaging focused predominantly on anatomical changes or gross inflammation. By targeting molecular processes underpinning radiation injury, ^18F-FAPI-04 PET/CT may enable clinicians to intervene earlier, possibly adjusting radiation doses or implementing protective measures before irreversible esophageal damage occurs. Furthermore, this technique might serve as a valuable tool for monitoring therapeutic responses and tailoring personalized treatment plans.
Technical aspects of the study underscore the benefits of ^18F-FAPI-04 as an imaging agent. Compared to conventional PET tracers such as ^18F-FDG, which highlights glucose metabolism, ^18F-FAPI-04 offers higher specificity for fibroblast activation and may reduce false positives related to non-specific inflammation or infection. Its favorable pharmacokinetic profile allows for clear imaging contrasts, facilitating precise quantification of tissue involvement.
While the study’s cohort size was moderate, the rigorous prospective design and comprehensive serial imaging add credibility to the findings. Nevertheless, larger multicenter studies are warranted to validate these results and establish standardized imaging protocols. Additional research could also explore correlations between ^18F-FAPI-04 uptake and histopathological markers of fibrosis and tissue remodeling.
This innovative imaging modality opens promising avenues beyond esophageal cancer; since fibroblast activation is a hallmark of many fibrotic diseases and radiation-induced injuries throughout the body, ^18F-FAPI-04 PET/CT may have wide clinical applicability. Its use could transform monitoring of radiation toxicity in other malignancies like lung or head and neck cancers, where esophagitis or mucositis is similarly problematic.
The integration of ^18F-FAPI-04 PET/CT into oncology practice aligns with the growing trend towards precision medicine, where molecularly targeted diagnostics complement therapeutic interventions. By illuminating pathophysiological processes at a cellular level, such approaches enhance clinicians’ ability to anticipate complications, adjust treatments, and ultimately improve patient quality of life.
In conclusion, the study spearheaded by Hu and colleagues offers compelling evidence that ^18F-FAPI-04 PET/CT is not only capable of detecting radiation esophagitis but also quantifying its severity in LA-ESCC patients undergoing chemoradiotherapy. Changes in tracer uptake directly mirror fibroblast activation prompted by radiation injury, serving as a non-invasive biomarker with potential clinical utility. Future advancements may cement its role as a standard tool for early diagnosis and management of this debilitating condition.
This innovative leap in functional imaging redefines the boundaries of cancer care diagnostics, emphasizing the critical interface between molecular biology and imaging technology. As this field advances, multidisciplinary collaborations will be essential to harness these insights towards tailored therapies and better outcomes for esophageal cancer patients worldwide.
Subject of Research: Detection and severity assessment of radiation esophagitis in patients with locally advanced esophageal squamous cell carcinoma using ^18F-FAPI-04 PET/CT imaging during concurrent chemoradiotherapy.
Article Title: Detecting radiation esophagitis using ^18F-FAPI-04 PET/CT in patients with LA-ESCC treated with concurrent chemoradiotherapy.
Article References:
Hu, X., Han, C., Zhang, M. et al. Detecting radiation esophagitis using ^18F-FAPI-04 PET/CT in patients with LA-ESCC treated with concurrent chemoradiotherapy. BMC Cancer 25, 854 (2025).
Image Credits: Scienmag.com
DOI:
Tags: 18F-FAPI-04 PET imagingassessing severity of radiation-induced damagecomplications of radiotherapy in cancerconcurrent chemoradiotherapy for LA-ESCCearly detection of radiation esophagitisesophageal squamous cell carcinomafibroblast activation protein imaginginnovative imaging techniques in cancer treatmentmolecular imaging agents in oncologynon-invasive monitoring of esophageal inflammationoncology imaging advancementsradiation esophagitis detection








No Comments
Leave a comment Cancel